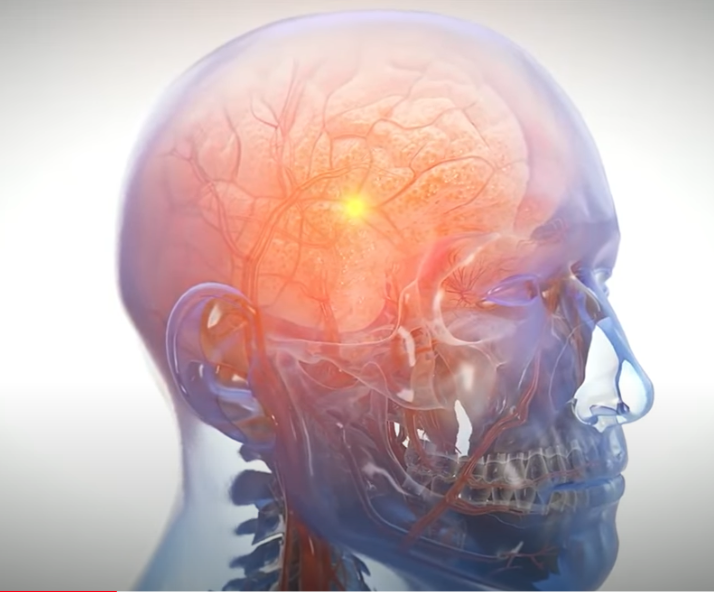
Football is a high-contact sport. Players accept some risk of injury every time they step out on the gridiron. However, it has only recently emerged that extended time playing football could increase a player’s risk of brain injury and brain disease substantially.
Chronic traumatic encephalopathy (CTE) has long been linked to football. What many experts did not know until recently was just how much more likely playing football makes developing CTE. The link between football (specifically tackle football) and CTE is very strong.
According to Boston University, every year that a football player spends on the field increases that player’s risk of developing CTE by 30 percent. In other words, the risk of developing CTE doubles every 2.6 years of play.
In addition:
- For players with possible CTE a diagnosis, the odds of developing severe symptoms of CTE doubled for every additional 5.3 years of football play;
- Those who played tackle football for more than 4.5 years were 10 times more likely to develop CTE than players who spent a shorter time in the sport; and
- Athletes who played football no more than 4 years have been diagnosed with CTE.
Interestingly, the same study found no link between CTE risk or severity and:
- Participation in contact sports outside of football;
- A player’s race; or
- The presence of other diseases.
In this blog post, we take a deeper dive into CTE risks for today’s football players. If you have questions about your legal rights in connection with a potential CTE diagnosis from playing football, contact an experienced brain injury attorney today for a free case evaluation.
An Overview of Chronic Traumatic Encephalopathy (CTE)
What is CTE?
Chronic traumatic encephalopathy is a progressive degenerative brain disease. Doctors believed it is caused by repeated head trauma, though medical experts have not yet identified exactly how repeated head trauma contributes to the significant brain changes that characterize CTE.
The brains of deceased athletes, especially those who played football and ice hockey, frequently exhibit signs of CTE.
How is CTE diagnosed?
Currently, doctors can only diagnose a possible or probable case of CTE in a living patient when a patient with a history of repeated head traumas also shows symptoms typical of neurodegenerative diseases (including ALS, Alzheimer’s, and Parkinson’s). However, doctors can only make a definitive CTE diagnosis by dissecting a person’s brain after that person has died. Medical professionals currently cannot use MRI, CT, or any other brain imaging methods to diagnose CTE.
How does CTE affect the body?
Since CTE is a degenerative brain disease, it slowly degrades the health of brain tissue over time, interfering with brain function. Medical experts believe that CTE causes sections of the brain to atrophy, or waste away. Our brains rely on nerve cells to conduct electrical impulses, communicate with each other, and keep our bodies functioning. People with CTE experience an interruption in communication between these cells.
Potential Causes of CTE
Repetitive brain trauma is, at present, the only definitive risk factor for developing CTE. It was once thought that CTE was only caused by repeated traumatic brain injuries, such as suffering repeated concussions. However, medical professionals now believe that even a history of microtraumas to the brain—damage so minor that the victim never experiences apparent symptoms—can lead to a patient developing CTE.
Repeated brain trauma has the potential to cause the brain’s tissue to degenerate. In most CTE patients, doctors find that over time, build-ups of a protein called tau begin to form in the brain, forming a telltale pattern that allows forensic pathologists to diagnose CTE after a patient dies.
The revelation that even microtraumas can lead to the development of tau formations and CTE has caused alarm because it means that a wide range of activities could lead to CTE even when participants take the safety precaution of wearing a helmet and/or noise protection.
These include:
- Participating in full-contact sports like football, hockey, boxing, mixed martial arts, and lacrosse;
- Participating in medium contact sports like soccer, basketball, and water polo;
- Serving in military roles combat commonly exposed to concussive blasts (such as explosions or artillery fire);
- Performing in work or recreational activities in which exposure to loud noise and/or extreme vibration is common, such as operating a jackhammer, driving a race car, or operating the soundboard for a touring heavy metal band.
In fact, the findings suggest that a wide range of mid and late-life cognitive and emotional decline could have some connection to CTE; far more than previously imagined. To learn more about football safety review our football helmet myths post.
Symptoms of CTE
To make matters more complicated, there are currently no known symptoms unique to CTE, which is why doctors cannot presently diagnose CTE in live patients. Over time, researchers hope to find signature markers of CTE that they can identify in living patients. For now, however, the diversity of brain injuries and how people experience them mean that common symptoms of CTE are also heavily associated with other conditions and brain traumas.
People with proven CTE (that is, people who have passed away and been diagnosed post-mortem) exhibited symptoms such as:
- Cognitive impairment (difficulty thinking);
- Emotional instability;
- Executive dysfunction (difficulty planning, carrying out tasks);
- Apathy, depression;
- Impulsive or aggressive behavior;
- Short-term memory loss;
- Substance abuse; and
- Suicidal thoughts or actions.
CTE symptoms don’t develop right after an injury. Medical professionals currently believe that the symptoms of CTE develop over time following repeated head trauma.
The symptoms and effects of CTE can contribute to tragic outcomes for patients and others around them. The case of the NFL football player Aaron Hernandez is a signature example of the devastation that CTE may cause. Hernandez had a bright-but-volatile career on the field, which ended when he was convicted of murder. He took his own life in prison at the age of 27. An autopsy later revealed that he suffered from an extreme case of CTE, with brain degeneration so severe that his brain resembled that of known CTE patients more than twice his age.
When to See a Doctor About CTE if You Played Football
Anyone who believes they have or be at risk of CTE should visit their doctor as soon as possible. Current and former tackle football players, in particular, should seek immediate medical attention for:
- Any blow to the head, even if it was not accompanied by any concussion symptoms like dizziness, confusion, or momentary loss of consciousness;
- Memory or cognitive problems, which can signal a potential degenerative brain disorder; or
- Depression or suicidal thoughts. Anyone with thoughts of self-harm can get help, 24/7/365, by calling the national suicide prevention hotline at 800-273-8255.
Football and CTE: Risk Factors
Playing tackle football inevitably involves taking repeated blows to the head and body. Current research suggests that these repeated blows, alone, could substantially increase football players’ risk of developing CTE.
However, doctors also know that not everyone who suffers repeated hits to the head develops CTE, and they continue to work to identify specific risk factors that might make developing CTE more likely in some players and not others.
Length of exposure to head impacts
Researchers believe that the longer the period of exposure to repeated head impacts, the greater the risk of developing CTE. Experts who study the link between CTE and football have found that the number of years playing football is a stronger predictor of the presence of CTE in a player’s brain than the number of concussions a player suffered.
Age at initial exposure to head impacts
Researchers also believe that the younger a player is when he or she first begins playing a contact sport, the greater the risk of developing CTE compared to other players in the same sport. Some studies indicate that exposure to impacts before the age of 12 constitutes a particularly significant risk factor for CTE.
CTE vs. Post-Concussion Syndrome
The growing awareness of CTE risks in football players has led to some confusion between that condition and the symptoms some players experience after suffering a concussion.
A concussion is a traumatic brain injury. A blow or jolt to the head can, essentially, rattle the brain inside the skull, damaging tissue, blood vessels, and nerves. Football players who suffer concussions in taking a hit often display a range of symptoms soon afterward, including loss of consciousness, dizziness, confusion, and nausea.
Concussion symptoms may resolve in a matter of hours or days, but some players continue to experience symptoms that persist for weeks, months, and even years. Doctors refer to this persistence of concussion symptoms as post-concussion syndrome.
To be sure, concussions and post-concussion syndrome are serious health conditions for which any football player should seek immediate medical treatment. However, post-concussion syndrome is not the same thing as CTE. Although researchers believe there is a strong link between suffering concussions while playing football and developing CTE, experiencing concussion symptoms, even long-lasting ones, does not mean a player has or will ever have CTE.
The acute symptoms of a concussion and post-concussion syndrome relate to the actual damage done to the brain by the blow a player takes to the head. This can heal with proper treatment. CTE symptoms, in contrast, are thought to result from the long-term deterioration of brain tissue associated with CTE.
The Risks of CTE Misdiagnosis
CTE is not verifiable until somebody has died. So, when someone has symptoms that could point to CTE, they must also remember that those symptoms might also indicate a wide variety of other mental health issues unrelated to CTE.
Misdiagnosis of CTE, in otherwise, can pose its own danger to a football player by distracting the player from seeking medical care for the actual condition causing symptoms. Former football players who experience CTE-like symptoms should never simply assume their brain has begun to deteriorate because of their football career. Instead, they should seek expert medical advice to rule out the vast array of other potential causes, many of which doctors can treat successfully.
Treatment for Football Players With CTE
Currently, there is no known cure for CTE.
Until a cure emerges, treatment for CTE will involve symptom management.
- Treating mood changes and emotional struggles. A football player who experiences mood changes and/or emotional due to CTE may find some relief through psychotherapy, mindfulness and meditation, and medication prescribed by a psychiatrist.
- Treating memory and cognitive challenges. Players can alleviate some memory and cognitive difficulties associated with CTE through brain training exercises, getting proper rest and nutrition, and maintaining overall mental and physical health.
- Treating headaches. Many CTE patients struggle with debilitating headaches. Fortunately, a wide variety of treatments exists for headaches, ranging from medications and massage to craniosacral therapy.
Preventing CTE in Football Players: Concussion Protocols Are Essential for Players at All Levels
As discussed above, researchers now believe that CTE can develop in football players who suffer repeated microtraumas, not just those diagnosed with multiple concussions. With that said, concussion protocols nevertheless represent an important means of minimizing the risk of football players developing CTE. Best practices that keep players safe from concussions generally help to keep them safe from other head trauma, too.
The NFL Head, Neck, and Spine Committee is a board of independent and NFL-affiliated physicians and scientists. They developed the NFL Game Day Concussion Diagnosis and Management Protocol in 2011. It is reviewed every year to ensure it prioritizes player safety to the highest degree possible.
The NFL’s Concussion Protocol lays good groundwork for protecting players at all levels of organized football from head trauma during practices and games.
The NFL’s Concussion Game Day Checklist
When a player takes impact to the head, the player goes into the Concussion Protocol if:
- The player reports or exhibits signs suggestive of a concussion or nerve pinch injury; or
- The team Athletic Trainer, booth ATC spotter, team Physician, NFL game official, coach, teammate, sideline Unaffiliated Neurotrauma Consultant (UNC), or booth UNC initiates the protocol.
Players who go into the Concussion Protocol must be removed from the football game entirely.
They need to go to the sidelines if possible or emergency medical professionals need to stabilize them on the field so that they can undergo the concussion assessment.
The sideline survey: After removing a player’s helmet, the Team Physician and Sideline UNC perform the sideline survey in a medical tent. A normal sideline survey and benign video allow a player to return to play. If any elements of a sideline survey are positive, suspicious, or inconclusive, the player must be escorted to the locker room;
- No-gos; cannot return to play: Confusion, amnesia, gross motor instability, LOC
- History of event
- Concussion signs and symptoms
- Maddock’s questions
- Video review
- Neurological exam: Cervical spine, speech, gait, eye movements, etc.
The locker room exam: If the locker room exam produces a normal assessment, the player can return to play. The Team Physician/UNC/ATC or the Team Physician/UNC performs the locker room exam. If any part of this exam is abnormal, the player cannot return to play;
- Complete NFL SCAT
- Complete neurological exam
Periodic evaluation by the medical team while the player stays in the locker room, follow-up neurological exam.
Concussion Protocol Improvements

The NFL’s Concussion Protocol received a handful of updates to improve player safety:
- Addition of a third UNC: Monitors broad video and audio from all feeds from the spotter booth notify UNCs on the field of a potential neck, head, spine injuries
- Defined impact seizure and fencing responses as independent No-Go criteria
- Required evaluation for players demonstration gross motor instability (like stumbling) to determine the root cause
- Teammates, officials, and coaching staff must take injured players directly to a medic team member
- All players who undergo concussion evaluations on game day must receive follow-up evaluations the next day
If you played football or other sports at any level and believe you may have developed, or risk developing, CTE, then you may have a legal right to compensation.
Contact an experienced brain injury attorney today to learn more.